|
|
|

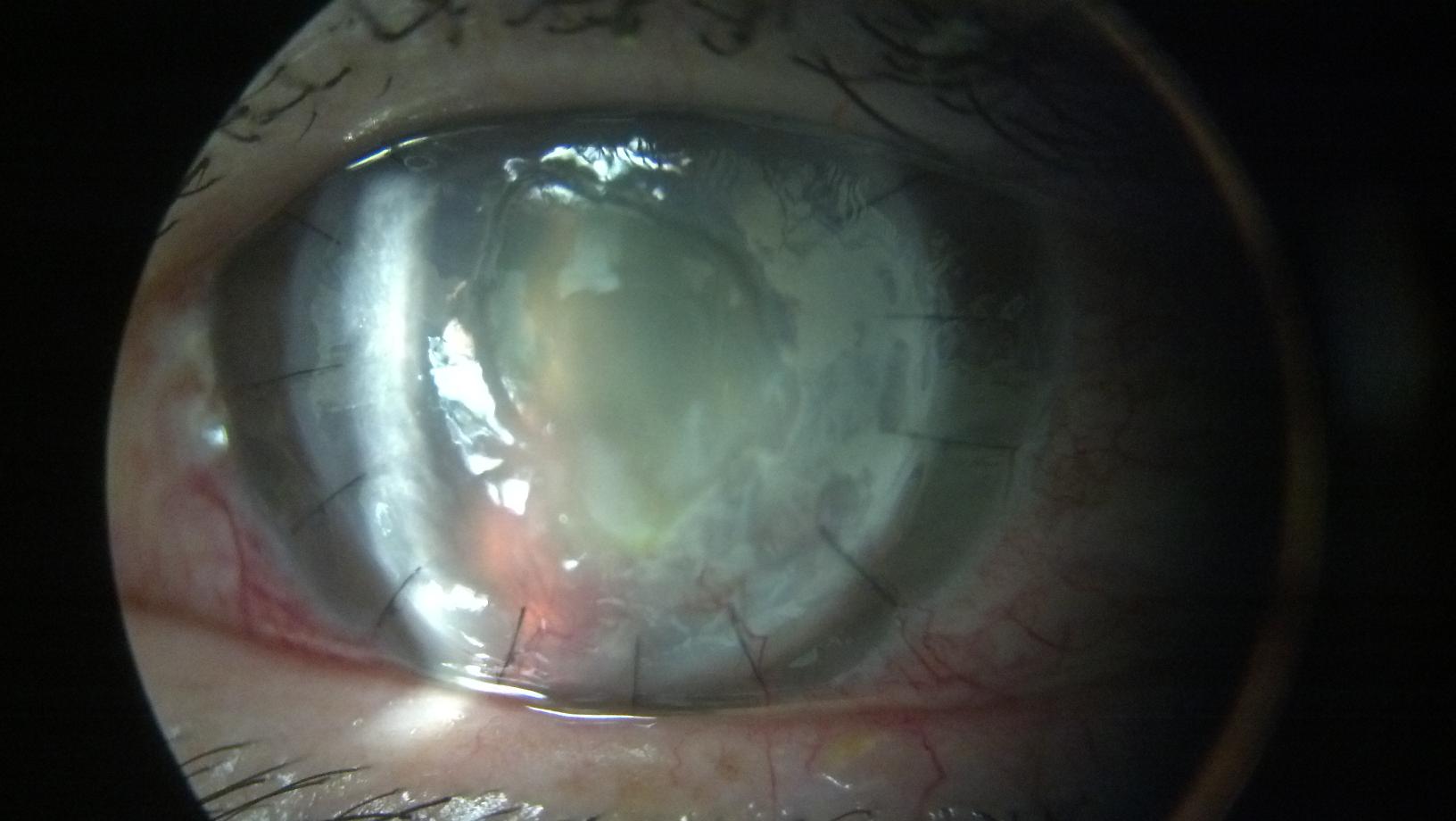
Operating microscope view of cornea with fungal keratitis and impending perforation,
which warrant action. However, when the patient’s immune state is heightened, traditional transplants can be compromised.
Slit lamp photograph of VisionGraft cornea with central epithelial defect. A dense cataract can also be noted. Sterile graft helps ensure long-term success
For situations involving a high risk of graft rejection, VisionGraft sterile tissue (Tissue Banks International, Baltimore) is a stopgap measure ultimately preserving long-term results, according to Gustavo A. Corrales, MD, Vision Consultants and Surgeons, Falls Church, Va. One of the biggest advantages of this gamma-irradiated sterile tissue is that it shouldn’t cause sensitization of the immune system, Dr. Corrales explained, adding that this tissue is devoid of any living cells that could trigger an immune memory.
In addition to cases such as lamellar keratoplasty or Boston type 1 keratoprosthesis surgeries, Dr. Corrales views the sterile tissue as ideal for situations where practitioners have an emergency. An example may be a situation where a patient has an infection of the cornea that is not responding to medical treatment or has perforated and needs to be taken to the operating room right away. “Then you have a red, inflamed eye; the whole immune system is revved up,” he said, adding that the quandary is you have to do something, but with the immune state heightened this may compromise long-term results. “Traditionally, we have put in a fresh cornea, but what we’re sacrificing is the long-term benefit because the immune system is going to get sensitized to this fresh corneal tissue,” he said. “It’s going to start rejecting the cornea and when you put the second one on this, it rejects as well.” For every new cornea, the chances of survival will diminish, he said.
A temporary solution
On the other hand, in transplant cases where the immune system is not revved up, such as keratoconus, chances of graft survival are high. This is about 73% at 10 years versus an emergency situation such as a corneal melt, infectious keratitis or trauma, where graft survival may be down around 40%, Dr. Corrales said.
The VisionGraft sterile tissue, which has no living cells for the immune system to detect, is not a target of the immune system. “You have time to decrease the inflammation, and after 6 months to a year when you have full control of the situation, you can go back and do another corneal transplant,” Dr. Corrales said. The VisionGraft tissue is not meant to be a permanent solution. It doesn’t have an endothelium and can get somewhat cloudy with time, even though no obvious edema develops. But during the transplant period, it can allow the patient’s immune system to quiet down enough to then give a traditional graft a much better chance of survival, he said.
VisionGraft in action
Dr. Corrales cited a recent case involving an uncontrolled diabetic patient who was referred to him with a very advanced corneal ulcer. The problem had begun about a month earlier when some vegetation had gotten into the 50-year-old patient’s eye while he was mowing the lawn.
By the time he came to Dr. Corrales’ practice, the patient’s visual acuity was limited to hand motions. At the slit lamp, the eye showed a stromal ring infiltrate, with an overlying epithelial defect that was 1.5 mm in diameter, as well as several satellite infiltrates; this turned out to be a fungal Aspergillus flavus infection. Even before the culture came in, suspicions were that this was a fungal case. “It was treated as fungal, but it was too late,” Dr. Corrales said. The ulcer unfortunately perforated, putting the eye in jeopardy. “We needed to do something immediately,” he said. “That’s when the idea of the VisionGraft came up.” Using an 8.75 mm VisionGraft cornea, investigators performed a therapeutic penetrating keratoplasty. At the end of the procedure, the patient was given an intracameral injection of voriconazole to eliminate any remaining infection.
The temporary graft integrated well. At 6 months, practitioners decided to proceed with a traditional transplant. While the VisionGraft remained clear, the patient had developed a cataract during this period, Dr. Corrales said. A triple procedure removing the cataract, implanting an IOL, and proceeding with a fresh corneal transplant was performed. The fresh transplant in the now quiet eye did well, with no signs of rejection, more than a year after the transplant. “His cornea was clear the last time that I saw him,” Dr. Corrales said. The patient ended up with a visual acuity of 20/200 as a result of his diabetic retinopathy.
In addition to giving the eye a chance to quiet down, he believes that the sterile cornea may have been helpful in controlling any lingering infection since most organisms probably couldn’t survive on the VisionGraft.
Dr. Corrales hopes that practitioners take away from the case the realization that they do have options with this tissue, which can buy time.
Going forward, he thinks more people are going to use the sterile tissue. “It can be kept on the shelf in the operating room, so that if you need it, it’s right there in emergency cases,” Dr. Corrales said. “I think the research is going to continue. There are a few issues to solve but I think it’s an exciting future.”
Editors’ note: Dr. Corrales has no financial interests related to this article.
Contact information
Corrales: [email protected] |





Comments are closed